“RCTs are the gold standard.”
That’s the mantra we all know in clinical research, and it’s true.
Or rather, almost true.
Because when it comes to medical devices, that model starts to crack.
Devices live in a reality that’s dynamic, operator-dependent, and constantly evolving.
Recognizing when an RCT isn’t the right choice doesn’t mean lowering the bar: it means raising the bar for scientific relevance.
Why RCTs don’t always fit
RCTs work beautifully for drugs: one molecule, one placebo, two well-controlled groups.
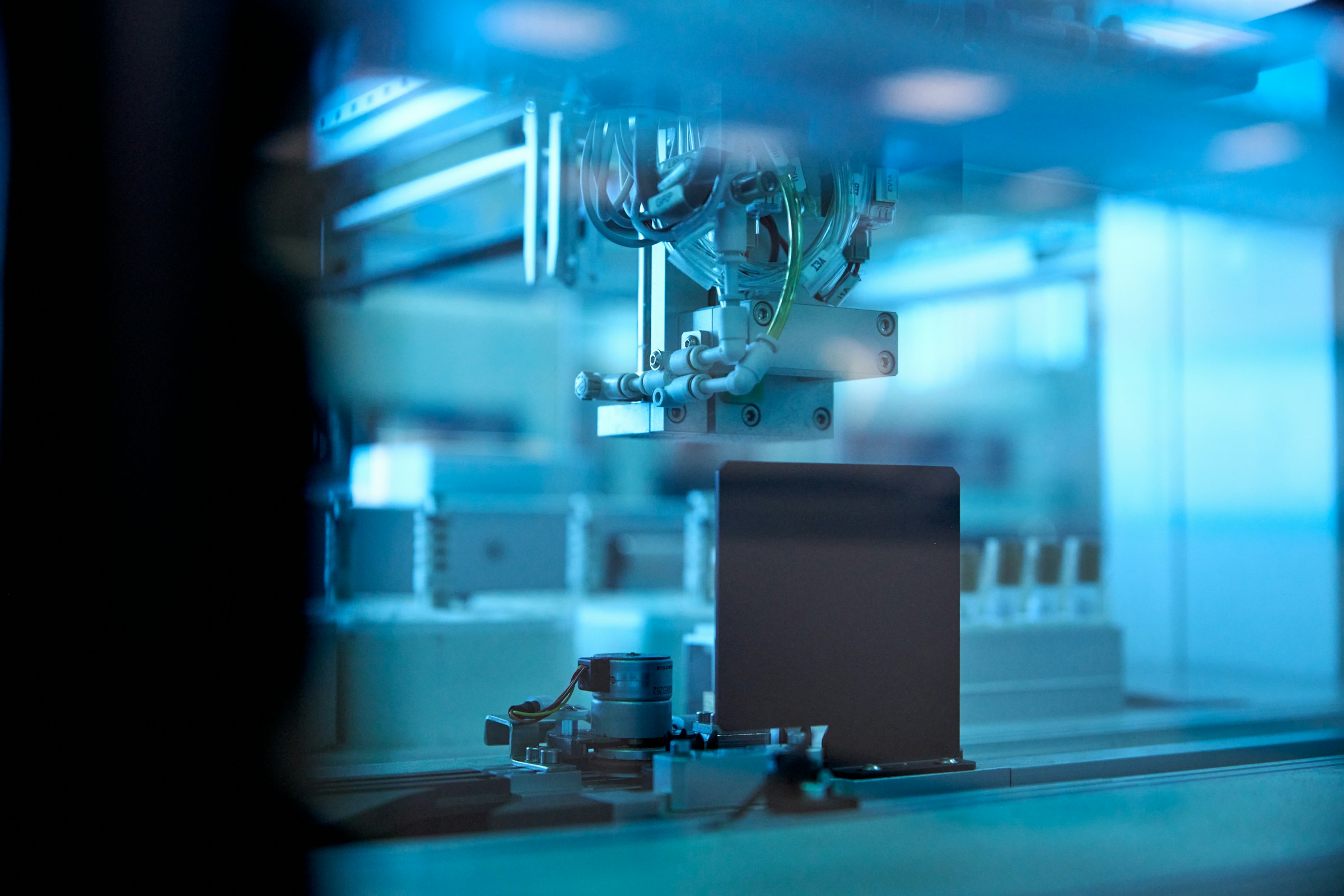
But devices aren’t pills: they’re tools that interact with people, techniques, and systems. And that makes all the difference.
Here’s why the “gold standard” can fall short:
- Learning curve: outcomes depend on user experience. A new robotic tool performs differently as expertise grows.
- Rapid innovation: by the time an RCT ends, the device might already have a new version.
- Small or niche populations: randomization isn’t always feasible or ethical.
- Blinding limitations: you can’t “mask” a surgical tool or software interface; bias will always exist.
So instead of asking “Can we randomize?” we should ask “Is this the best way to answer the question?”
The “fit for purpose” approach
Both FDA and European regulators now recognize that what matters isn’t symmetry: it’s scientific coherence.
The right question isn’t “Is this an RCT?” but “Is this design fit for purpose?”
Here’s what that can mean in practice:
- Cohort studies: well-structured, prospective designs to track long-term performance.
- Registries and RWD: large, real-world datasets that, when well managed, support strong evidence.
- Pragmatic or observational studies: reflecting actual clinical practice, not idealized conditions.
- Historical or synthetic controls: leveraging existing data transparently when randomization isn’t possible.
Each of these designs can deliver evidence that’s relevant, robust, and proportionate to the device’s risk and purpose.
Choosing the right design
Selecting a study design isn’t about templates: it’s about reasoning.
It starts with a clear understanding of the clinical question, technology maturity, and regulatory expectations.
Ask yourself:
- What are we really trying to prove: efficacy, safety, usability, or performance?
- Would randomization clarify or distort results?
- Where is the device in its lifecycle: early-stage or established?
- What data already exist and how can they be leveraged responsibly?
Both FDA and MDR guidance emphasize the same principle: rigor lies in justification, not format.
Beyond methods: how we think about evidence
For years, “non-randomized” sounded like “less rigorous.”
Today, it can mean more relevant.
A well-designed observational or hybrid study isn’t a compromise: it’s a conscious, justified, transparent choice.
Because in medical device research, quality doesn’t come from rigidity, but from reasoning.
At We4CR, we believe scientific quality starts with the right design, not necessarily the most traditional one.
That’s why we partner with investigators to define strategies that meet both regulatory standards and real-world needs.
Because clinical research shouldn’t just follow rules, it should make sense.
Not sure if an RCT is truly the best fit for your study?
Ask our team of experts: we’ll help you find the most effective and compliant design 👉 https://l.we4cr.com/j-7l
Already running an RCT?
Make sure your study stays rock-solid with our tools for data integrity and quality management: https://new.we4healthcare.com/solutions/set-up/